By Dr. Adam Vascellaro, D.O., CPN Chief Medical Officer
I suspect many would not have expected we would be in November and still right in the middle and on the front lines of a worldwide COVID-19 pandemic. Unfortunately, it is still very real, while getting closer to our homes and work every day. In fact, here in Oklahoma we’re consistently among the top states for record-setting numbers of new cases. I’m sure by now those of you reading are in the same place I am — knowing multiple patients, coworkers and family who have recently battled the illness. Thankfully, most infected have been able to remain at home with only symptomatic medications, socially-distanced support and faith. Some of you may even know one patient included in the approximately 5 percent whose symptoms became severe enough to require hospitalization. COVID-19 hospitalization is scary, not only medically, but even more so from a humanistic perspective. Typically, these patients are hospitalized in order to receive supplemental oxygen and other supportive-type care. They commonly require treatments utilizing BIPAP, ventilators, lung bypass machines and dialysis. The humanistic challenge is that your family member is hospitalized and in quarantine. Their only — and possibly final — means of communication with loved ones being an impersonal phone or FaceTime call.
It has been a struggle throughout the pandemic to balance giving the information necessary to convey the reality of the virus and generate a need for people to act cautiously in their interactions and activities, while not inciting fear.
The following chart included here shows how the pandemic has been progressing within Citizen Potawatomi Nation Health Services. I believe CPNHS data generated without political bias is a very good sample of what is truly going on in Oklahoma. This chart goes from February to October 2020. It clearly shows that not only are we still in the “first wave” of the pandemic but also that it is not slowing down.
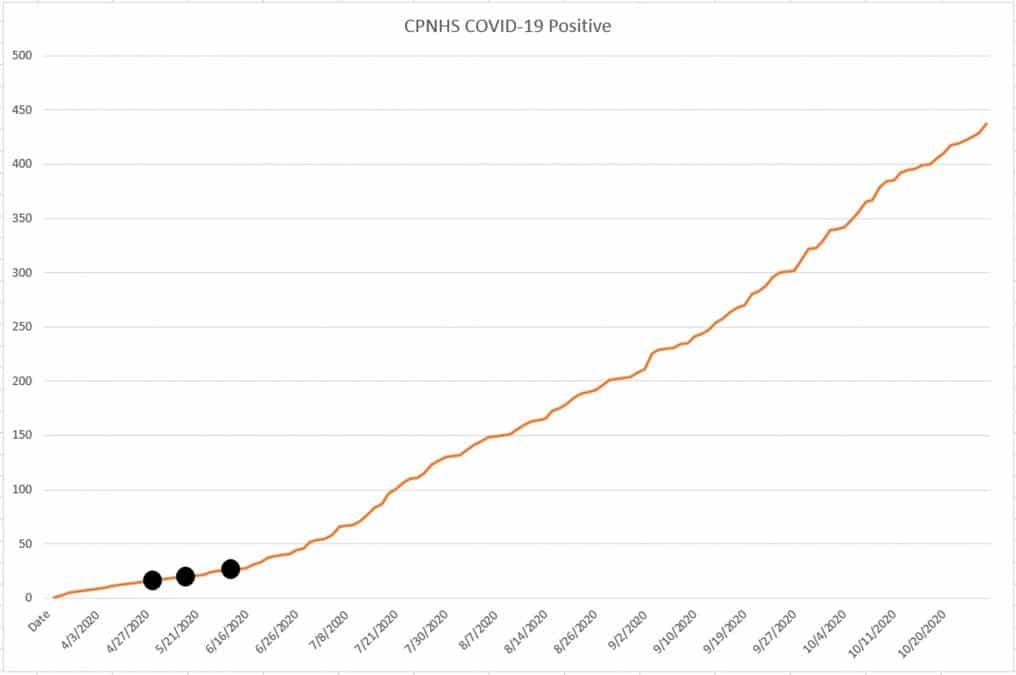
Please pay specific attention to the three black dots added to the line on the chart. They represent the dates of the State of Oklahoma’s three “reopening” phases that all took place without a statewide mask mandate. I personally think the pandemic is spreading fast and will continue to do so, potentially with greater death rates, if people in our state and communities don’t start practicing appropriate mask wearing and social distancing. Mask mandates are needed in our cities, counties and state.
I am grateful to Tribal Chairman John “Rocky” Barrett for showing true crisis leadership, making the unpopular decision based in part on CPNHS’ internal COVID-19 real-time testing data to implement a mask mandate throughout the Citizen Potawatomi Nation. He did so at the same time that the state government and other local leaders in Oklahoma were unwilling to do what is needed and right. Much of the criticism of his decision cited political opinions partially based upon the biased, flawed data generated from the State of Oklahoma, which at the time did not include antigens testing.
CPN and the surrounding communities are at the crossroads of multiple hot spots. If you were to draw a line from the recent COVID-19 hotspots of Norman to Stillwater and another one from Seminole to McLoud, the junction point and area surrounding it is the Tribal jurisdiction and areas CPNHS serves.
If the state and local communities don’t start insisting on social distancing and mask mandates, I anticipate things will get far worse. Respiratory viruses like COVID-19 tend to have more severe symptoms in the winter months. Adding in the potential for contracting Influenza A along with the virus, there is a rising concern that patient’s symptoms will be much more severe than what has occurred during the summer months. As such, we are highly recommending all CPN patients get their flu shots as soon as possible!
You keep hearing that Oklahoma hospitals have plenty of ICU beds and ventilators, which is probably true. What you are not hearing is that the staff of a 24/7 ICU with three shifts of nurses is growing more and more strained. There are limits on the number of qualified staff to man these wards, and the state’s hospitals are especially short of lung bypass machines, also knowns as EMCOs. Patients are placed on these when high flow oxygen and ventilatory support isn’t enough. CPNHS’ first patient was on ECMO at Integris in Oklahoma City. Shortly thereafter, another of our patients had to be sent to a Tulsa hospital for ECMO. Just a couple of weeks ago, another of our patients had to be sent to Baylor University Medical Center in Texas in order to get ECMO treatment. The concern is there are limited, or possibly no more, ECMOs available in Oklahoma right now. This may be a preview of other strains on in-patient resources that will become noticeable to those of you outside the medical field.
An additional unfortunate reality with hospitalization is the bill that comes with it. A $10 mask may be inconvenient or uncomfortable, but it may be preferable to a very steep hospital bill following an extended stay in the ICU.
CPNHS and CPN are well ahead of the curve in containing the spread of COVID-19 as well as the methods proven to operate safely through it. CPNHS is a leader in real-time COVID-19 PCR testing. By combining it with COVID-19 IgG antibody testing, we have aided our decision makers to allow policies approving the return of COVID patients to work or school on a case-by-case basis. This stands in stark comparison to the U.S. Centers for Disease Control and Prevention’s semi-educated, always changing and politically biased, one-size-fits-all recommendations.
Tribal Emergency Management Director Tim Zientek and his staff are actively leading and collaborating with local civic leaders to prepare for multiple COVID-19 immunization drives on an unprecedented scale in our communities. Our health services anticipates having access to two separate vaccines in the near future. The first is expected to be the BioNT/Pfizer vaccine currently slated for a January 2021 release and the Moderna vaccine currently estimated for mid-2021. Both are two-shot vaccines with 21 days between the doses.
A yet-to-be-determined priority will determine who get the vaccines first. Frontline health care workers, first responders, and high-risk patients will be first priority, followed by the general population.
Again, CPNHS and Oklahoma are in the midst of a worsening first wave. I hope that we can keep playing defense long enough to get to herd immunity between spreading infection and upcoming immunizations so we can get there with minimal physical and social casualties. We have a long way to go and a short time to get there.
I am praying for all.
