Kaitlyn Precure will not be eating a cheeseburger any time soon, thanks.
Because of an allergy to red meat, that cheeseburger could cause the Potawatomi Leadership Program alumna to start swelling or break out in hives.
“I figured it out about two years ago,” she said. “After eating red meat a couple of times, especially roasts with lots of fat, I’d swell up.”
An allergy is when the body’s immune system overreacts to a substance that would normally be harmless. In Precure’s case, it was in response to a tick bite she received as an adult.
Although a food allergy and a food intolerance can cause nausea and diarrhea, and both require avoiding certain dishes, they are not synonymous. The latter usually stems from the body’s inability to break down a food, Oklahoma City Indian Clinic pediatrician Dr. Jennifer Stewart said.
“People are allowed to have preferences but this does not constitute an allergy,” she said. “A true food allergy is only present in 8 percent of children and most of them will eventually be outgrown.”
After consuming an allergen, the body’s immune system releases a host of chemicals, including histamines, which stimulate the nerves and cause blood vessels to dilate, and leukotrienes, which cause inflammation. That in turn can lead to a wide array of bodily reactions, such as hives; a rash; swelling of the hands, feet or tongue; wheezing; blurred vision; nausea; or a tingling tongue, face or lips.
An allergy can be life threatening if an individual ingests enough of the substance to trigger anaphylaxis, which constricts the airways and prompts blood pressure to plummet, causing the body to go into shock.
A suspected allergy confirmation, whether it is to food or other substances, can occur either through a blood test, which looks for antibodies to the allergen, or through a skin prick test. This includes rubbing a small amount of the suspected allergen into the skin to see if it causes hives or a rash.
In the case of food, positive results to either test can be further verified by eating some of the substance in question while medical professionals look for signs of an allergic reaction and, if needed, provide medical intervention. Over-the-counter testing is available, but as Stewart pointed out, it does not always yield accurate, dependable results.
“The over-the-counter food allergy testing is not reliable and does not tell you if your child actually has an allergy or sensitivity to a food,” she said. “All of us have some degree of antibodies to food proteins but this does not mean we are allergic to the food. If you simply feel bad after eating a particular type of food but do not have an immunoglobulin-mediated response to that food, you are not allergic.”
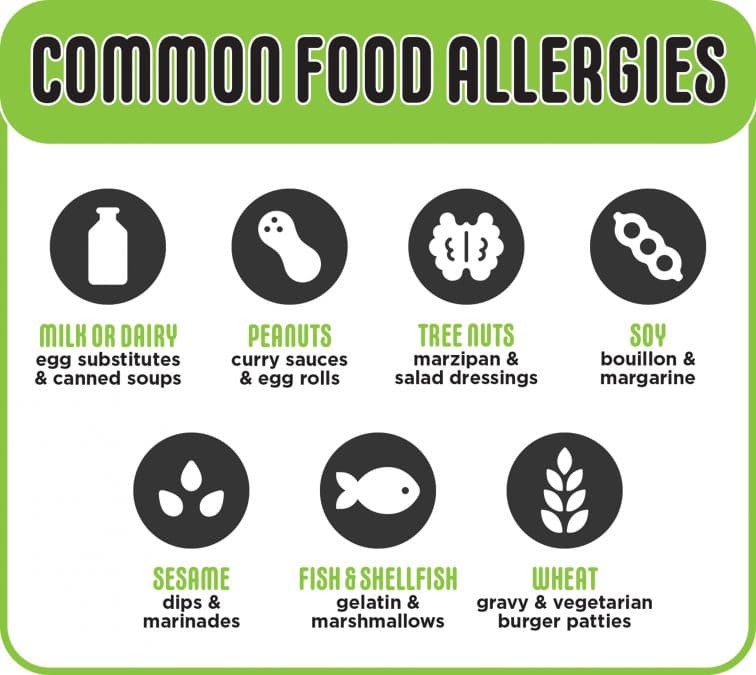
More than 170 foods have been connected with allergic reactions, with the most common ones being milk, eggs, peanuts, tree nuts, shellfish, soy, wheat, fish and sesame.
According to Harvard Women’s Health Watch, food allergies are more common among people who have other allergies, eczema, asthma or hay fever.
Despite the prevalence of diagnoses increasing by 377 percent between 2007 and 2016, demographic data on the roughly 32 million food allergy patients is limited. However, according to a study published in March 2020 of more than 23 million children nationwide receiving Medicaid benefits, Native American children were 24 percent less likely than their white peers to have a diagnosed food allergy.
Despite noting that it impacts about 1 in 10 adults nationwide, a 2019 study on the severity and prevalence of food allergies on adults did not include Indigenous people in its methodology.
The author of both studies, Dr. Ruchi Gupta, acknowledged that those Medicaid families may not have the same access to allergy specialists and may attribute allergic reactions to something other than what is in their pantries, thus leading to an undercount in the data set.
“I see it in my own clinic,” she said, while presenting on a panel during the Food Allergy Research and Education Global Summit in October. “My patients don’t always tell me about food allergies. They’re sometimes focusing more on other issues, like asthma.”
Meanwhile, for Precure, a descendent of the Beaubien family, confirmation that her hives were an allergic reaction meant slightly changing her diet.
“In a way, this has been a good opportunity for me. It’s made me learn about new recipes and trying new things,” she said.
“I used to have the mentality that all my protein had to come from meat. I’m now including more alternative sources, like lentils and beans.”
